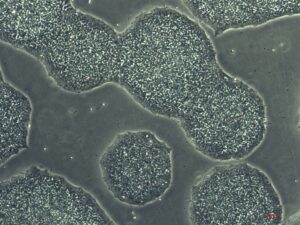
The unique nature of induced pluripotent stem cells (iPSCs) lies in their capability for unlimited self–renewal and programmed differentiation into virtually any adult cell types [1]. iPSC based technology holds the potential to treat a multitude of diseases and conditions, ranging from neurodegenerative disorders like Parkinson’s and Alzheimer’s disease to heart diseases and spinal cord injuries [2,3]. The differentiation potential of iPSCs allows researchers and medical professionals the ability to study cell-type specific disease mechanisms, discover novel biomedical therapies and develop personalized treatments.
Unlike conventional pharmaceutical therapies that offer a “one-size-fits-all” approach, iPSC-based therapies using autologous cells from each patient can be customized to target the underlying disease while preserving the unique genetic makeup of each patient. This personalized approach helps to minimize the risk of immune rejection and enhance the efficacy of the therapy. This level of personalization holds immense promise for improving patient care and outcomes across various medical conditions.
Even though multiple clinical trials using iPSCs are ongoing worldwide [4], the technology still faces many (technical) challenges in obtaining high-quality reliable cells for therapy. These include reprogramming efficiency, expansion, differentiation capabilities and quality control, all hampering the development of high-quality iPSC products [5]. Furthermore, concerns regarding teratoma formation [6], mutagenicity and epigenetic changes remain relevant as this technology moves closer to clinical practice.
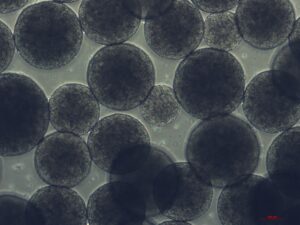
SCINUS is actively focusing on solving the technical challenges in generating high-quality reliable iPSCs for various clinical applications, drug screening and disease modelling. In the first edition of our new ‘Ask the Expert’ series, our Process Development Engineer Juda-El Sam will share her work on developing protocols for iPSC expansion using the SCINUS bioreactor, and the specific challenges associated with this cell type. Stay tuned!
References
[1] Medvedev SP, Shevchenko AI, Zakian SM. Induced Pluripotent Stem Cells: Problems and Advantages when Applying them in Regenerative Medicine. Acta Naturae. 2010 Jul;2(2):18-28. PMID: 22649638; PMCID: PMC3347549.
[2] Stoddard-Bennett T, Reijo Pera R. Treatment of Parkinson’s Disease through Personalized Medicine and Induced Pluripotent Stem Cells. Cells. 2019 Jan 7;8(1):26. doi: 10.3390/cells8010026. PMID: 30621042; PMCID: PMC6357081.
[3] Nagoshi, Narihito, Hideyuki Okano, and Masaya Nakamura. “Regenerative therapy for spinal cord injury using iPSC technology.” Inflammation and regeneration 40 (2020): 1-5.
[4] Kim JY, Nam Y, Rim YA, Ju JH. Review of the Current Trends in Clinical Trials Involving Induced Pluripotent Stem Cells. Stem Cell Rev Rep. 2022 Jan;18(1):142-154. doi: 10.1007/s12015-021-10262-3. Epub 2021 Sep 16. PMID: 34532844; PMCID: PMC8445612.
[5] Sangbae Park, Yonghyun Gwon, Shahidul Ahmed Khan, Kyoung-Je Jang, Jangho Kim. Engineering considerations of iPSC-based personalized medicine. Biomater Res. 2023;27:67.DOI:10.1
[6] Gutierrez-Aranda, Ivan, et al. “Human induced pluripotent stem cells develop teratoma more efficiently and faster than human embryonic stem cells regardless the site of injection.” Stem cells 28.9 (2010): 1568-1570.
Cheng, Yang, et al. “Artificial intelligence technologies in bioprocess: opportunities and challenges.” Bioresource Technology 369 (2023): 128451.
SCINUS is actively focusing on solving the technical challenges in generating high-quality reliable iPSCs for various clinical applications, drug screening and disease modelling.
